
Correction of deformities and limb lengthening
Correction of deformities and limb lengthening
LDeformities of the limbs, resulting from deviations from normal anatomy or changes in the length of bone segments, can be caused by congenital, metabolic, tumour-related, or high-energy trauma-induced fractures with or without bone loss.
Surgical techniques are employed for the surgical treatment of limb deformities, allowing correction of axial deviations, replacement of lost bone segments, and potentially limb lengthening.
Correction requires a bone osteotomy, which serves as the pivot for axial deviation correction.
Bone regeneration can occur through repair after a fracture or bone section (osteotomy) performed in the operating room, followed by gradual distractive traction, allowing the formation of new bone tissue (osteogenesis). This way, bone segments can be gradually corrected and/or lengthened to bridge any bone gaps.
Choosing the right site for osteotomy and the correction method is crucial. The following approaches can be used:
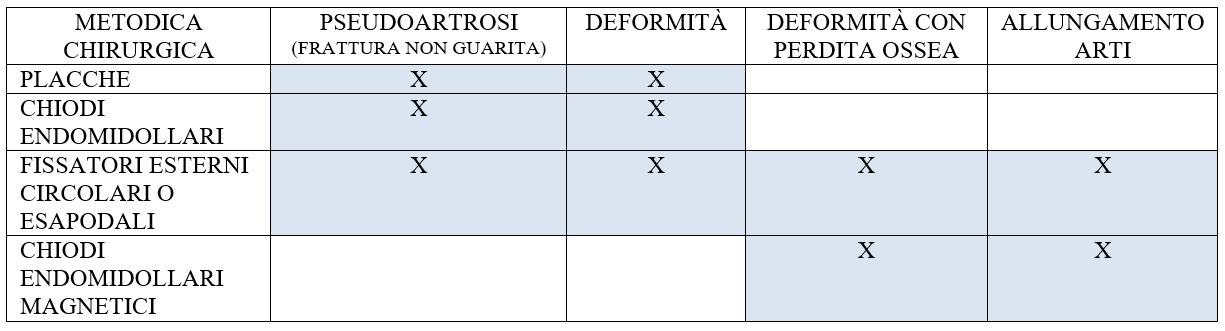
- A surgical open technique involving only osteotomy and stabilisation with a plate or intramedullary nail can be applied in cases of simple malunion or pseudoarthrosis.
- The use of circular or hexapodal external fixators allows bone regeneration using the principle of osteogenic distraction. They are more versatile and can be used in almost all bone pathologies, including fractures (especially in open and complex fractures). The downside of these fixators is the extended application time, during which the patient wears a c
- For lengthening a simple bone segment or those with mild axial deviations, extendable intramedullary nails, using magnetic impulse, have been introduced in recent years but remain relatively expensive.

Osteogenesis by distraction
Osteogenesis by distraction was pioneered in 1951 by Professor Gavril Abramovich Ilizarov, a Russian physician who first developed a circular external fixator for fracture treatment. After numerous applications of this fixator, Ilizarov realised that it not only facilitated the healing of fractures when kept stable and aligned but also allowed bone lengthening by distraction. Ilizarov demonstrated that with controlled tension, bone and soft tissues could be reliably and reproducibly regenerated.
Bone section with periosteum preservation, followed by gradual separation of the two bone portions connected to the circular fixator, leads to progressive bone growth in the intervening zone at a rate that can reach up to 1 mm per day.
This method can be used to treat various pathologies such as:
Lower limb densitometry
Lower limb disparity can result from congenital, developmental, post-traumatic, or post-surgical causes.
Post-traumatic disparity occurs due to improper bone healing after a fracture, leading to a shorter limb.
The treatment objectives are to correct the disparity with associated deformities, preserve the function of muscles and joints, and restore normal limb alignment.
Post-traumatic bone deformities
Post-traumatic bone deformities are fractures that heal in a displaced, angled, rotated, or shortened position. This malunion can be challenging to treat, especially with polyaxial alterations, involving deformities in multiple planes (e.g., rotational defects associated with varus or valgus). In such cases, the use of hexapodal external fixators is highly recommended. These fixators employ computerised preoperative planning, allowing the gradual correction of deformities with the aid of specific programmes.
Pseudoarthrosis (non-healed fractures)
A late complication resulting from the disruption of normal fracture healing processes leads to pseudoarthrosis. This may be associated with limb disparity, infections, and joint stiffness. In addition to axial deviations, there will be difficulty in bone healing, coupled with fracture instability. The surgical technique must, therefore, involve:
a. Mechanical stabilisation of the pseudoarthrosis site
b. Restoration of biology (ensuring well-vascularised bone tissue)
c. Correction of any axial deviations
Bone tissue loss due to tumours, trauma, and infections
Tumours, trauma, and infections can result in the loss of bone mass due to soft tissue injury associated with fractures, infectious processes, or resection of bone segments for bone or soft tissue tumours. This loss can lead to a significant bone defect, resulting in limb disparity.
Joint contractures
Joints can be limited in their movement by contracted muscles or periarticular scars due to trauma.
Bone infection
Bone infection can result from a fracture or a bloodstream infection (usually occurring during childhood). The only effective way to remove bone infection is to resect the bone portion affected by the infectious process. This can cause a bone defect that must be reconstructed using the Ilizarov technique.
Preoperative visit
A preoperative assessment involves a detailed examination of the medical history and a review of previous X-rays. Specific X-rays and often a Computerised Tomography (CT) scan and/or Magnetic Resonance Imaging (MRI) evaluation are needed to complete the assessment.
If surgical treatment is deemed appropriate, all aspects of the procedure are discussed with the patient. A follow-up appointment is then scheduled to address further questions and establish a definitive treatment plan. It is crucial for the patient to understand what can realistically be achieved through surgery and the possible complications.
Surgical procedure
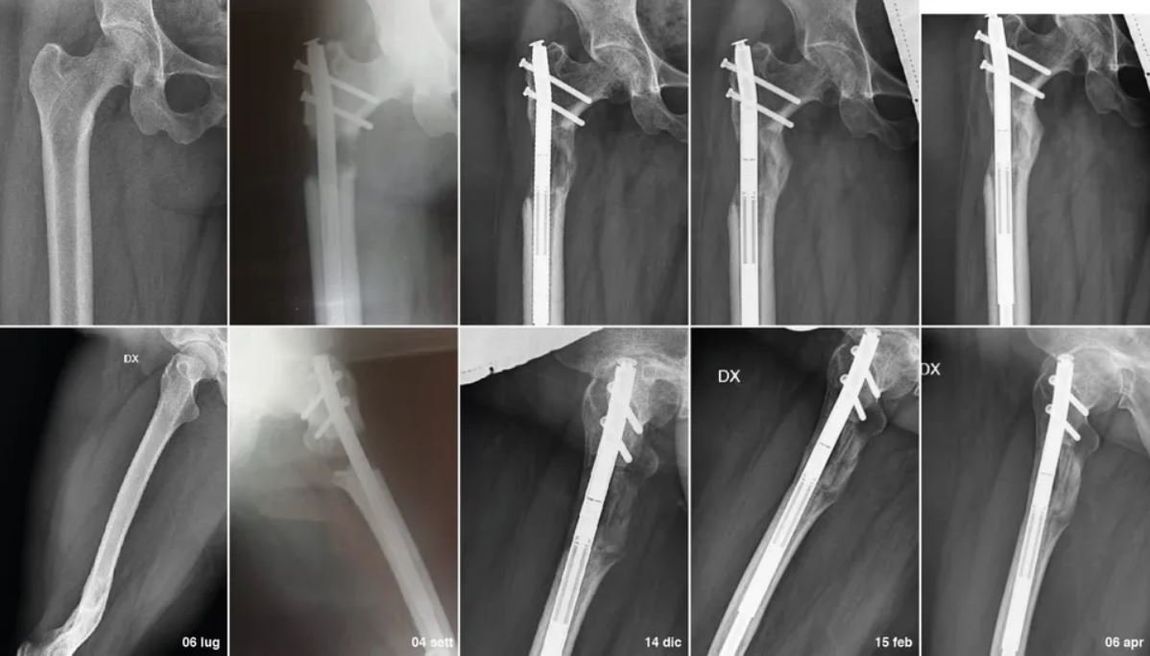
Intramedullary nail and plates
The insertion of an intramedullary nail or open plating is performed after a thorough study of the deformity. In the case of deformities that do not require bone lengthening, these will be monitored with serial postoperative checks every month until bone consolidation is achieved.
Magnetic intramedullary nail fo lengthening
In the case of a magnetic intramedullary nail for lengthening, the patient is equipped with a device that sends a magnetic signal for nail lengthening. This procedure is performed every evening until the desired lengthening is achieved. Monthly checks are then required for the assessment of bone consolidation, and once consolidation is achieved, the removal of the nail can be scheduled, usually after about 6 months of bone consolidation.
Circular or hexapodal external fixator
In preparation for each surgical procedure, a personalised device is prepared. The external circular structure of this device is surgically connected to the affected limb using steel wires and pins (screws). Surgery is usually performed percutaneously through small incisions. Specialised bone incisions are made with particular care to minimise damage to surrounding bones, soft tissues, nerves, and blood vessels.
Adjustment phase
In general, patients are hospitalised for 5-7 days before being discharged. More complex procedures may require a longer hospital stay.
The actual lengthening and correction (straightening) of the limb begin approximately 5 days after the surgical procedure. At this point, the apparatus is adjusted according to a plan provided based on a personalised computerised program given to the patient postoperatively. The patient must adjust the length of the millimetre rods placed between the rings every day according to the provided schedule. The bone ends of the osteotomy are thus gradually moved apart at a predetermined speed, usually ranging between 0.5 and 0.7 mm, to achieve gradual bone regrowth.
Since muscles do not lengthen as easily as bones, physiotherapy is an essential step in the treatment to maintain joint mobility and prevent contractures. Once the initial wound healing has occurred, 5-7 days after the procedure, free ambulation can begin, with the apparatus being medicated three times a week and kept clean using disinfectant to clean the rings and pins. Subsequently, the patient is visited every 30 days with blood tests and X-rays.
Strict monitoring of soft tissues and pin tracts must be maintained to identify any complications.

Consolidation phase (bone hardening)
After the desired length is achieved, and bone deformities are corrected, adjustments to the apparatus are stopped to initiate the consolidation phase.
The apparatus is then left in place, and consolidation usually takes place in 5-6 months.
Once the new bone is deemed sufficiently strong, the apparatus is completely loosened, and the patient is encouraged to fully weight-bear for two weeks. If this can be achieved without compromising proper healing, the removal of the apparatus is scheduled. This occurs in the operating room, using mild sedation for the patient.
After removing the external fixator to protect the newly formed bone, a plaster cast or brace is usually applied. Over time, the new bone tissue will regain all the qualities and strength of normal bone, allowing for the complete functional recovery of the treated limb.
Follow-up
Regular follow-up appointments are crucial to monitor the ongoing recovery and address any emerging issues. These appointments involve thorough assessments, including clinical examinations and imaging studies, to ensure the sustained success of the treatment and the patient's overall well-being.
Relief from pain
The initial postoperative phase after the application of the external fixator can be painful, but it is moderated by pain-relieving medications administered in the ward. After the first 3 or 4 days of pain, the body gets accustomed to the presence of the external fixator, and the pain diminishes until it disappears at rest. The return of pain occurs with the first weight-bearing steps and the adjustment in lengthening of the rods because they stimulate the muscles acting near the metal pins.
The adjustment phase proves to be painful due to the continuously changing conditions of the bone and soft tissues. After the lengthening period, the pain decreases until it almost disappears.
The perceived pain remains quite subjective but is usually well tolerated with adequate pain management.
Care of wires and screws
It is possible to shower with the Ilizarov apparatus once the wounds are dry, usually 5 days after surgery. It is advisable to clean the wound areas once a day using an antibacterial solution, such as 0.05% Chlorhexidine, and cotton wipes. Sometimes, a soft toothbrush may be necessary to clean up a crust buildup that can often form around the wounds. Do not be alarmed; it is entirely normal, a biological reaction of the body to the presence of an external body with a metallic tract exiting the skin. The body tries to heal itself and close the hole from which the pins emerge.
Some patients may experience serous leakage from one of the exit holes of the pins.
Once again, do not be alarmed; this can be entirely normal. If this occurs, immerse a piece of Lyofoam® in an antibacterial solution (e.g., Chlorhexidine) and apply it to the wound. If you notice that one of the wounds starts to have a more reddish colouration, it is necessary to contact the treating doctor or the doctor overseeing the external fixator.
When the wounds have stopped secreting fluid and appear clean and dry, they can remain uncovered.
Smoking
It is possible to shower with the Ilizarov apparatus once the wounds are dry, usually 5 days after surgery. It is recommended to clean the wound areas once a day using an antibacterial solution, such as 0.05% Chlorhexidine, and cotton wipes. Sometimes, a soft toothbrush may be necessary to clean up a crust buildup that can often form around the wounds. Do not be alarmed; it is entirely normal, a biological reaction of the body to the presence of an external body with a metallic tract exiting the skin. The body tries to heal itself and close the hole from which the pins emerge.
Some patients may experience serous leakage from one of the exit holes of the pins.
Once again, do not be alarmed; this can be entirely normal. If this occurs, immerse a piece of Lyofoam® in an antibacterial solution (e.g., Chlorhexidine) and apply it to the wound. If you notice that one of the wounds starts to have a more reddish colouration, it is necessary to contact the treating doctor or the doctor overseeing the external fixator.
When the wounds have stopped secreting fluid and appear clean and dry, they can remain uncovered.
Possible complications
Complications can occur during the lengthening period, fixation, or after the removal of the apparatus.
Complications are usually divided into two types: biological (infections) or mechanical.
Biological:
Superficial wound infection: treated with antibiotics
Delayed bone consolidation: intervention involves slowing or stopping the lengthening rate
Mechanical:
Deformity of the regenerated bone: easily corrected with the application of external hinges without the need for invasive procedures
Mobility defects:
easily corrected with adjustment of the apparatus screws
Muscle contractures and joint dislocations: treatable with physiotherapy
All these complications, except superficial infection, can also develop with intramedullary nails, but in the case of external fixation, they are better manageable. In case of infection of the intramedullary nail or plates, they must be removed, and another intervention is required after an adequate course of antibiotic therapy.








