Morton's neuroma
Morton's neuroma
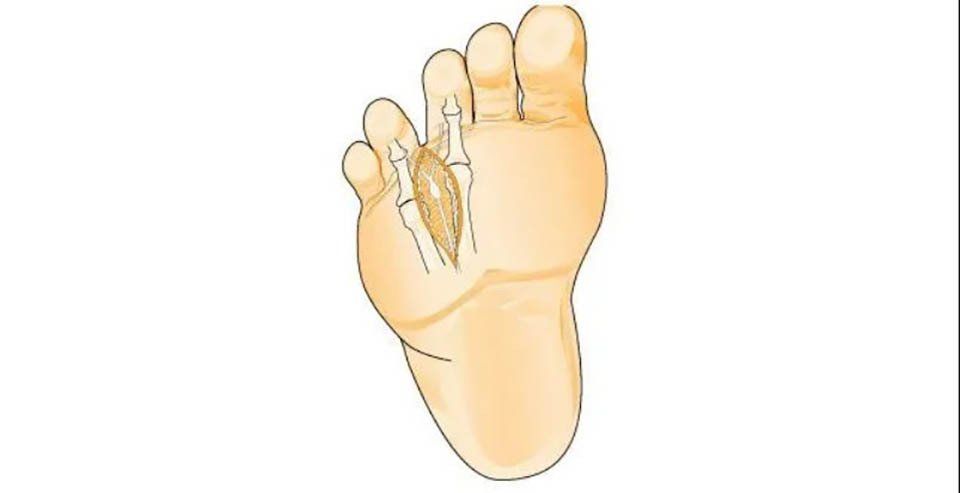
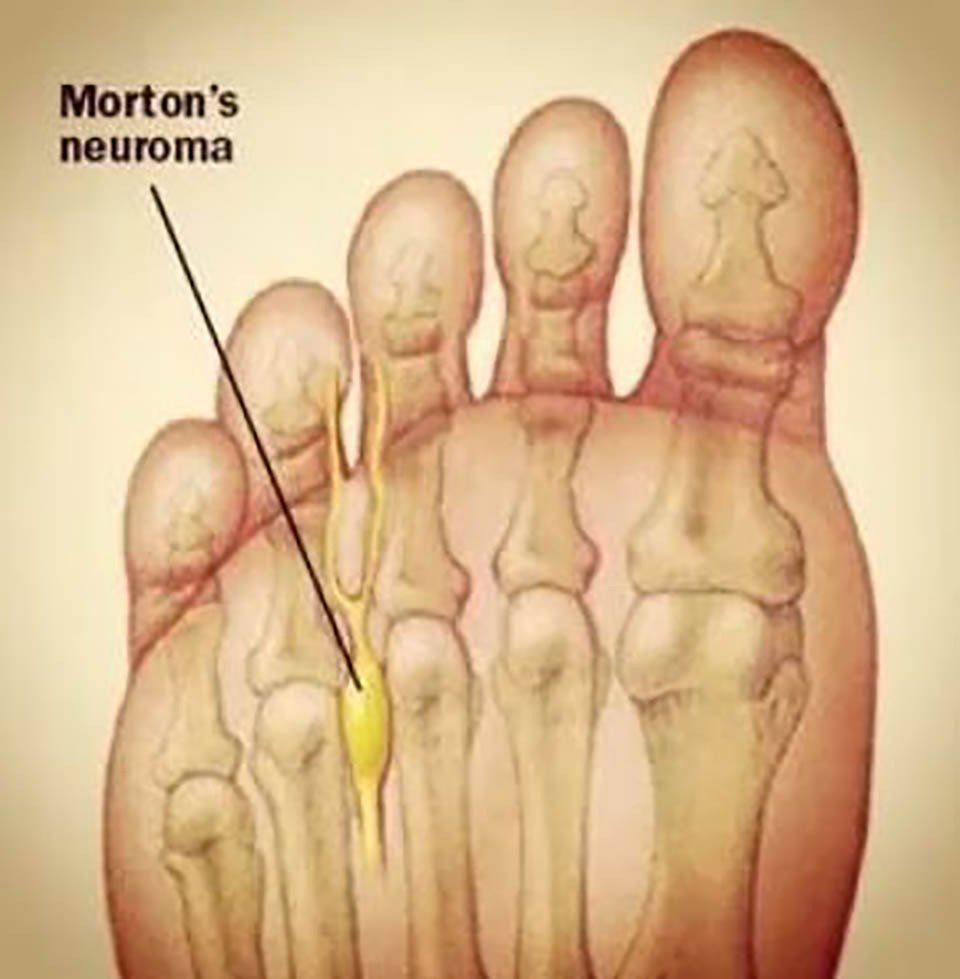
Morton's neuroma is a compression neuropathy (with associated perineural fibrosis) caused by the entrapment of the interdigital nerve near the distal edge of the transverse intermetatarsal ligament.
The second and third interdigital nerves in the forefoot are more commonly involved. Morton's Neuroma is more frequent in women. Patient history and physical examination are essential for diagnosis, and diagnostic imaging includes weight-bearing X-rays, ultrasound, and magnetic resonance imaging.
Most patients can be treated conservatively with footwear modification, custom orthotic use, nonsteroidal anti-inflammatory drugs, and cortisone injections.
Surgical treatment should be reserved for those patients who do not respond to conservative treatment.
Alternatives to surgery include percutaneous electrocoagulation, endoscopic decompression, cryogenic denervation, and injection of alcohol or phenol. The most commonly used surgical treatments are neurolysis, release of the intermetatarsal ligament with or without neurolysis, nerve resection, and intermuscular transposition of the neuroma.
Currently, there is no evidence regarding the best treatment for Morton's Neuroma. All literature reviews emphasize the need for more accurate studies to demonstrate the best treatment for this condition.
Definition
Morton's Neuroma is a non-neoplastic interdigital nerve compression disorder that causes associated neural degeneration and perineural fibrosis.
The most common theory for the pathogenesis of Morton's neuroma is mechanical compression. The intermetatarsal space is located between the two metatarsals, and within it are vessels and nerves that reach the toes. The structure that binds the two metatarsals is the transverse metatarsal ligament. In almost all cases, symptoms originate from the bifurcation of the common digital nerve and can extend to the toes.
The neuroma usually produces symptoms when it reaches a diameter of at least 4 mm. This condition predominantly affects adults in the third decade of life and is more common in females than males.
History
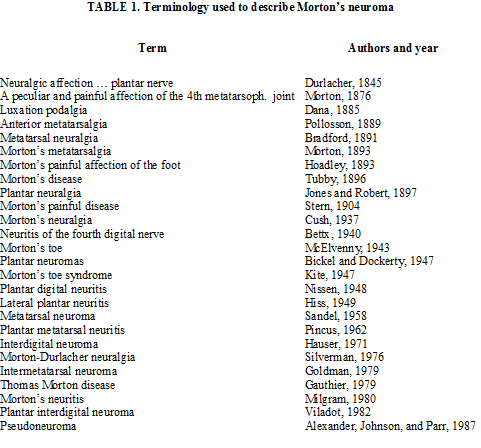
In 1835, Civinini, a professor of anatomy at the University of Pisa, was the first to describe the fusiform swelling of the third common digital nerve on a cadaver.
In 1845, Durlacher discussed the management of this painful condition but did not give it a specific name.
Heuter, in 1870, provided a description of Morton's neuroma treatment.
Then, in 1876, Thomas Morton clinically described "a specific painful condition of the fourth metatarsophalangeal joint."
Hauser and Williams discussed interdigital neuroma in their 1939 text titled "Foot Pathologies," and in 1940, Betts suggested that the cause of the pathology lies in the increased thickness of the third interdigital nerve.
Nomenclature
There are numerous conditions involving the interdigital nerves, and depending on the involved space, there is a different designation for the pathology.
Joplin was associated with a painful condition of the medial digital nerve of the hallux.
Heuter was associated with involvement of the 1st intermetatarsal space.
Hauser was associated with involvement of the 2nd intermetatarsal space.
Morton was associated with involvement of the 3rd intermetatarsal space.
Iselin was associated with involvement of the 4th intermetatarsal space.
In 1835, Civinini, a professor of anatomy at the University of Pisa, was the first to describe the fusiform swelling of the third common digital nerve on a cadaver.
In 1845, Durlacher discussed the management of this painful condition but did not give it a specific name.
Heuter, in 1870, provided a description of Morton's neuroma treatment.
Then, in 1876, Thomas Morton clinically described "a specific painful condition of the fourth metatarsophalangeal joint."
Hauser and Williams discussed interdigital neuroma in their 1939 text titled "Foot Pathologies," and in 1940, Betts suggested that the cause of the pathology lies in the increased thickness of the third interdigital nerve.
Pathological anatomy
The macroscopic appearance of neuroma is characterized by localized thickening with increased volume of the plantar digital nerve at the point of bifurcation into its digital branches. The neuroma looks similar to traumatic neuroma or neurofibroma; however, while Morton's neuroma is characterized by degenerative changes, neurofibroma is characterized by proliferative changes.
In this pathology, the involved interdigital nerve shows histopathological features divided into three stages:
- Initial phase: characterized by endoneurial edema and sclerosis of vascular walls.
- Central phase: characterized by fibrosis, endoproliferative sclerosis, and perineurial vascular pathologies.
- Final phase: characterized by endoneurial sclerosis, diffuse demyelination, and vascular obliteration.
There are various theories about the etiopathogenesis of Morton's Neuroma, all of which consider histopathology. These theories include the inflammatory process, neurofibroangiomatous tumor, ischemic injury, entrapment, neuropathy, and derivation from repeated microtrauma.
Entrapment neuropathy is often found in the third intermetatarsal space, where the nerve is relatively fixed, and significant shear forces are transmitted from the hindfoot to the forefoot. These forces, acting on the nerve, promote inflammation.
Symptoms
The patient's reported clinical history is usually characterised by numbness and tingling radiating to the toes. Pain is often localised on the plantar side in the intermetatarsal space and may be felt as a burning sensation.
There may also be a sensation of a new formation on the plantar side, with dysesthesias resembling the feeling of walking on a ball or something rough.
Symptoms may increase with weight gain, prolonged standing, the use of tight-toe closed footwear, and high heels. Usually, to alleviate pain and symptoms, the patient must remove shoes and massage the foot.
Clinical signs
The diagnosis of Morton's neuroma is made by analysing the patient's clinical history and performing clinical and instrumental tests. Toe deformities, cavus or flatfoot, and previous metatarsal osteotomies may be contributing factors, but they might not be implicated as the main causative factors of Morton's neuroma, which can also be of idiopathic origin.
The most used clinical tests are Mulder's sign, which is performed by compressing the forefoot transversely and simultaneously applying plantar and dorsal pressure with the other hand.
The positive result consists of a click, often painful for the patient, which can be felt by the doctor. Another useful test is Gauthier's test in which the forefoot is compressed, and medial and lateral pressure is applied.
Bratkowski described a test involving hyperextension of the toes and the examiner's thumb rolling in the symptomatic area. This manoeuvre can reveal, on palpation, a thickened longitudinal mass.
Morton's neuroma symptoms can be replicated through Tinel's sign and Valleix's phenomenon.
Careful palpation along the interdigital nerves is useful to determine the point where the nerve remains compressed and if other nerves are involved.
An injection of selective lidocaine under the intermetatarsal ligament at the pain site, which should bring immediate relief to ambulation, can be useful for confirmation.
Instrumental exams
Although the physical examination is highly predictive, for a more accurate diagnosis, instrumental exams must be necessarily used:
- Weight-Bearing X-rays: These should be regularly ordered to rule out skeletal pathologies, such as stress fractures and bone neoplasms, even if the neuroma will not be visible in X-rays.
- Ultrasound: It is used for the evaluation of the intermetatarsal space, and the neuroma will appear as an oval mass with hypoechoic signal. This mass will be parallel to the long axis of the metatarsals and is best observed in the coronal projection.
- Magnetic Resonance Imaging (MRI): It is very useful for diagnosis, although in the literature, it is indicated as in-depth diagnostic, which should be reserved for atypical presentations. However, we consider this method essential for a better definition of the size and location of Morton's Neuroma. The neuroma is detected in T1 sequences as a well-defined mass with low signal intensity.
Differential diagnosis
The possible clinical differential diagnosis of Morton's neuroma includes:
- Stress fractures of the 3rd or 4th metatarsal
- Transfer metatarsalgia
- Intermetatarsal bursitis
- Rheumatoid arthritis
- Autoimmune arthropathies
- Localised vasculitis
- Ischaemia
- Tarsal tunnel syndrome
- Metatarsophalangeal dislocation syndrome
- Metatarsophalangeal capsulitis
- Osteochondritis dissecans (Freiberg’s)
- Nerve root compression syndromes
- Peripheral neuropathies (Diabetes)
- Ganglion or synovial cysts
- Fibromyalgia and other chronic pain syndromes
Conservative treatment
Non-surgical treatment is based on reducing plantar pressure and nerve irritation. Initially, patients should wear shoes with a wide toe box to allow the metatarsals to spread.
The use of custom-moulded insoles leads to load distribution, especially useful in cases of functional overload.
Local anaesthetic and steroid injections can also be effective. Greenfield et al. presented a study that showed a clear improvement in symptoms in 30% of cases and a partial response in 50%.
However, caution must be exercised regarding the excessive use of corticosteroid injections: some studies describe the occurrence of plantar fat pad atrophy and skin discolouration secondary to cortisone injections.
Some authors report improvement with the use of injections with vitamin B12.
Minimally invasive operative treatments
- Percutaneous electrocoagulation
- Endoscopic decompression
- Cryogenic denervation
- Injection of alcohol or phenol
Surgical treatment
Several surgical techniques have been described for the treatment of Morton's Neuroma. The most commonly used ones are:
- Neurolysis
- Section of the intermetatarsal ligament with or without neurolysis
- Nerve resection
- Intermuscular transposition of the neuroma
1. Neurolysis
2. Section of the Intermetatarsal Ligament
The first to describe this procedure was Gauthier in 1979, who treated 304 neuromas with the section of the intermetatarsal ligament associated with neurolysis, achieving an 83% success rate in terms of symptom resolution. Subsequent authors have reported similar results.
Winfield performed the section of the intermetatarsal ligament without neurolysis with good preliminary results. In general, an 80% success rate is reported, with the advantage of preserving the nerve, allowing a quicker return to normal activities, although recurrences are not rare.
3. Nerve Resection
Four different surgical approaches are described in the literature for nerve resection:
a. Longitudinal plantar incision (Hoadley 1893) (Betts 1940)
b. Transverse plantar incision (Nissen 1948)
c. Interdigital incision (McKelvenny 1943)
d. Longitudinal dorsal incision (McKeever 1952)
Today, the two commonly used techniques are the longitudinal plantar incision and the dorsal incision.
A) The plantar approach involves a longitudinal plantar incision followed by the splitting of the plantar fascia to expose Morton's neuroma. The nerve is cut distally to its bifurcation and as proximally as possible. It is essential to release any branches of the interdigital nerve to avoid neuroma recurrences. Although the plantar approach provides good visibility, easy access to the entire neuroma, and leaves the intermetatarsal transverse ligament intact, some authors prefer it in case of revision. The disadvantage of this technique is a higher percentage of pain and irritation on the plantar side, along with a 3-week non-weight-bearing period.
B) The dorsal approach consists of a longitudinal skin incision on the involved intermetatarsal space, exposing the transverse intermetatarsal ligament and Morton's neuroma. This is removed with distal dissection of the nerve to its bifurcation and as proximally as possible. The advantages of this technique include a faster healing time compared to the plantar approach, and weight-bearing is allowed earlier. The disadvantage is the difficulty in exposing the entire nerve.
Foot surgery
4. Intermuscular Transposition of the Neuroma
This technique involves the resection of Morton's neuroma followed by the transfer of the proximal end of the nerve to an intrinsic muscle. Through a plantar approach, Wolfort achieved 80% excellent results with symptom relief, returning to regular work, and the ability to wear unrestricted footwear.
Complications
The main complications after Morton's neuroma treatment include numbness of the interdigital space, wound dehiscence, and recurrences. Difficulty in wearing footwear is reported in more than 70% of cases, especially with high heels.
To reduce the incidence of these problems, it is necessary to perform delicate tissue manipulation and meticulous haemostasis, followed by compressive dressing to prevent postoperative haematoma formation.
During the procedure, it is essential to identify the digital branches and the proximal trunk of the nerve to ensure complete lesion resection. It is important to cut the nerve as proximally as possible and be cautious not to damage the intermetatarsal artery and tendons near the intermetatarsal space.
Conclusion
Most authors emphasise the need for a thorough clinical history and examination. Crucial for a definitive diagnosis is the use of weight-bearing X-rays, ultrasound, and magnetic resonance imaging, which identify Morton's neuroma, assess its dimensions and location, aiding in choosing the best treatment.
Non-surgical treatment can be useful in some cases, leading to a reduction in symptoms. Literature reports over 80% satisfactory results after lesion excision, but complications are challenging to manage.
Currently, there is no evidence regarding the best treatment for Morton's neuroma. All literature reviews stress the need for more accurate studies to demonstrate the most effective treatment for this condition. However, we believe that a currently mini-invasive surgical approach (1.5 cm) dorsally represents the most effective treatment for this pathology, providing good visibility of structures and complete neuroma removal while avoiding damage to nearby structures.