Rearfoot surgery
Surgery of the hindfoot
Dr. Roberto Bevoni specialises in specialist surgery of the hindfoot and midfoot, treating post-traumatic pathologies, including cases with severe loss of bone substance.
Pathologies of the posterior foot are treated with both traditional and minimally invasive techniques.
Dr. Roberto Bevoni also deals with the treatment of flat feet in adults and children and high-arched feet.
Achille tendon
Inflammatory conditions and ruptures
Pain in the back of the leg can have various origins. Depending on its location and symptoms, it can be related to various pathologies. Vascular pathologies such as thrombosis are associated with forced immobilisation, which can occur in the case of fractures and traumatic injuries to the ankle and knee.
Its onset is sudden, usually not related to traumatic events and sports activities. Much more frequent are injuries that can be attributed to the musculoskeletal system.
The back of the leg is composed of 3 main muscles (the 2 gastrocnemius and the soleus) that fuse together to form the Achilles tendon. In the world of sports, the triceps surae is the most vulnerable muscle-tendon complex due to its high load-bearing capacity and some peculiarities.
Although injuries to the two gastrocnemius muscles due to contractions and muscle tears are commonly encountered in orthopaedics, the Achilles tendon represents the final and most vulnerable part of this system, which, by attaching to the heel, transmits force for movement to the ankle and other structures of the foot.
Pathologies affecting the Achilles tendon can also be present in non-athletic patients, with a higher frequency among diabetic, obese, and rheumatic individuals. However, sports activities have a strong correlation with the onset of Achilles tendon injuries.
In athletes, functional overloads due to overly intense training, too short rest periods, and inappropriate footwear can create micro-injuries, which, if repeated over time, can lead to the formation of chronic inflammation and rupture of the tendon.
There are also anatomical factors that make it more vulnerable. Firstly, the Achilles tendon does not have a synovialised sliding sheath but is contained in a split of the deep fascia of the leg. Additionally, there is an area about 4 cm from its insertion into the heel characterised by poor vascularity. Moreover, physiological ageing leads to progressive loss of elasticity, which, if associated with trauma or structural defects subjecting it to overload, leads to the onset of degenerative lesions.
The symptoms of tendon distress are quite clear. Commonly, there is pain in the back of the leg at the tendon or its insertion, which increases upon palpation. The tendon may increase in volume over time and become irregular to the touch, a sign of degeneration of its structure (tendinosis). Morning stiffness, if present, can be used as a parameter for assessing the severity of the injury, as it reflects the loss of elasticity of the degenerated tendon portion. Usually, in athletes, pain occurs during physical activity, disappearing at rest. If inflammation becomes chronic, it may begin with physical activity and limit the duration and intensity of exercise. Tendinitis is defined as acute if symptoms are present for less than two weeks, sub-acute from 3 to 6 weeks, and chronic if more than 6 weeks.
The most frequent location of the pathological process is in the body of the tendon (60%), followed by the insertion (25%), and the proximal part (15%).
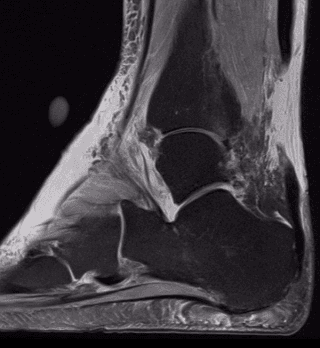
The diagnosis can be further explored with instrumental examinations such as ultrasound and magnetic resonance imaging.
Non-invasive treatment is the first approach to use in the case of Achilles tendon dysfunction. Rehabilitation associated with physical therapy can be helpful in relieving symptoms and, if well-conducted, can restore the tendon to normality in a good percentage of cases. However, in clinical practice, there is often a chronicisation of inflammation and pain or discomfort that persists over time, limiting the patient's physical activity.
If not treated promptly, this inflammation progressively leads to degeneration and rupture of the tendon, which the patient perceives as a snap in the posterior region, leading to functional impotence to lift the tip of the foot and inability to walk. In these cases, the patient experiences sudden pain that does not subside and worsens with walking; the only possible treatment is surgical.
In the case of tendon inflammation that does not subside, a non-surgical treatment is recommended, involving the infiltration of platelet-rich plasma (PRP) into the tendon body. This often yields good results in the case of body lesions.
Minimally invasive surgical treatments include tenolysis and scarifications, which aim to free the tendon from adhesions and eliminate the degenerated tendon portion, repairing any partial tears.
Tendon rupture
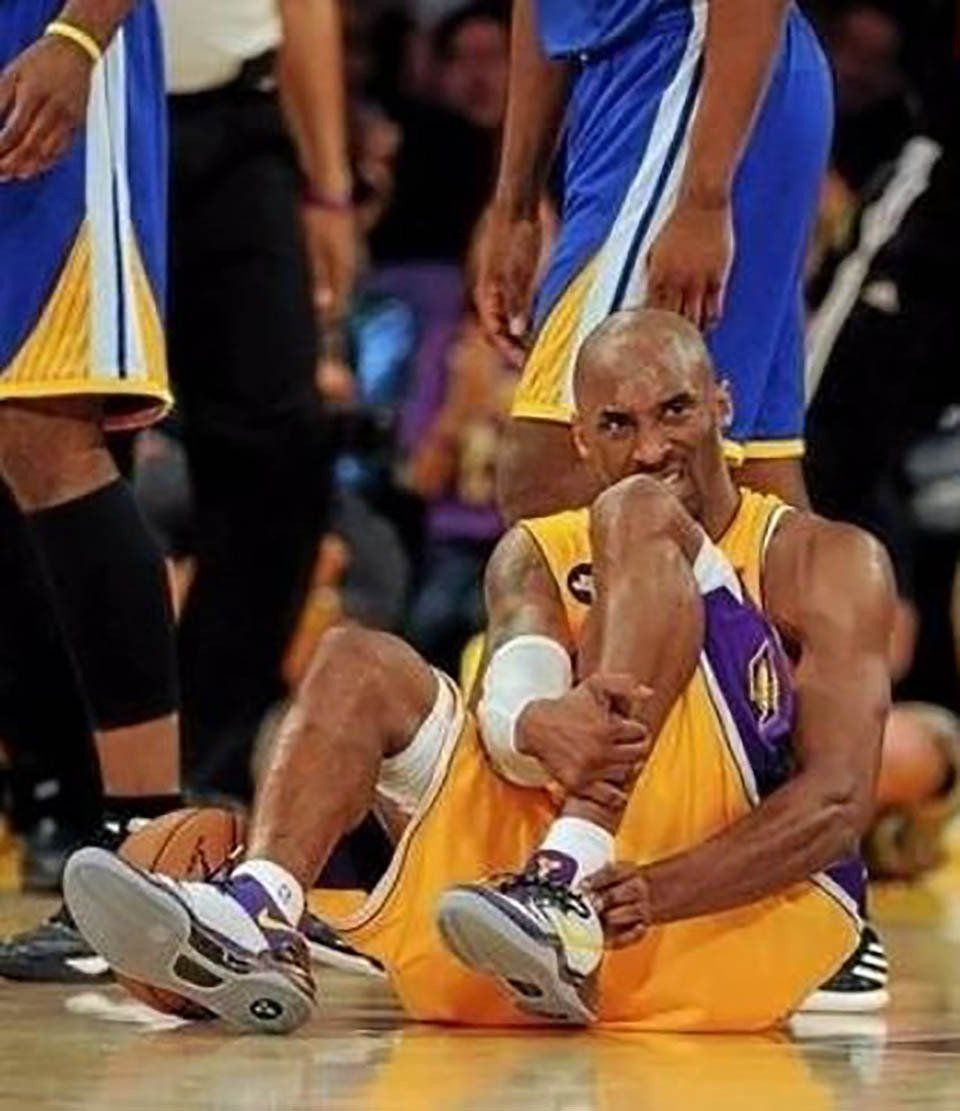
Tendon rupture is more frequent in males (M/F: 5/1) with a higher incidence between 30 and 50 years. Often, patients affected by this rupture are amateur athletes. The sports incident is the basis for rupture in 65% of cases; the remaining 35% can occur following twisting traumas or functional overloads in an already degenerated tendon.
The rupture is generally unilateral; bilateral ruptures are usually related to pathologies and predisposing factors such as hyperuricaemia, prolonged treatment with corticosteroids, rheumatoid arthritis, systemic lupus erythematosus, renal failure, hyperthyroidism, and prolonged treatment with fluoroquinolone antibiotics.
In most cases, the rupture is between 2 and 6 cm from the insertion into the heel, an area characterised by lower vascular supply. Clinically, a localised increase in volume at the leg can be observed, sometimes associated with bruising due to the haematoma resulting from the rupture. Palpation reveals the tendon interruption, with a depression at the site of the lesion.
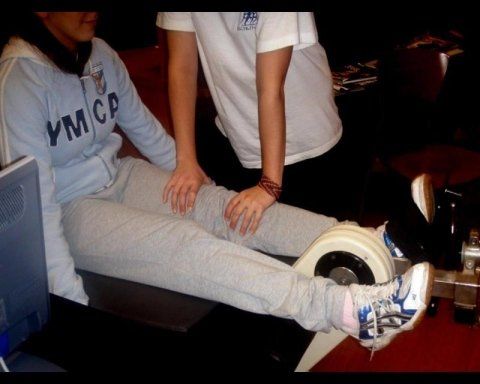
The Thompson or Squeeze test, performed by compressing the calf, yields a positive result, meaning that compression does not result in plantar flexion of the foot, a sign of tendon interruption. The patient cannot stand on tiptoe on the leg affected by the lesion, and a limp may be present, with a strength deficit during propulsion.
While the clinical diagnosis seems relatively straightforward and is often complemented by magnetic resonance imaging and ultrasound, it's essential to remember that in 20% of cases, this lesion goes unrecognised, leading to a worsening clinical picture due to tendon retraction, which progressively increases in the first 15 days following the injury.
Conservative treatments have been described even in the case of rupture, but the results obtained suggest considering treatment with a cast or functional bandaging only for individuals with reduced functional demands or severe concomitant pathologies. This is due to a higher percentage of tendon re-ruptures and a decrease in strength and functionality of the non-surgically treated tendon when compared to the results of those treated with surgical repair.
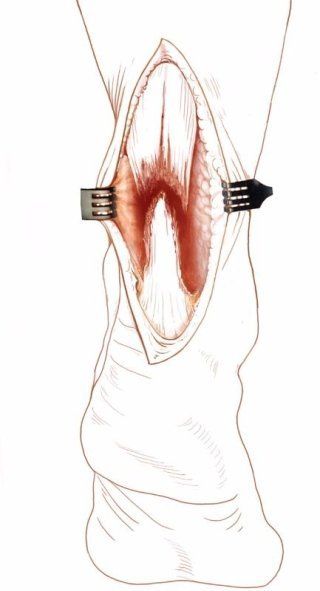
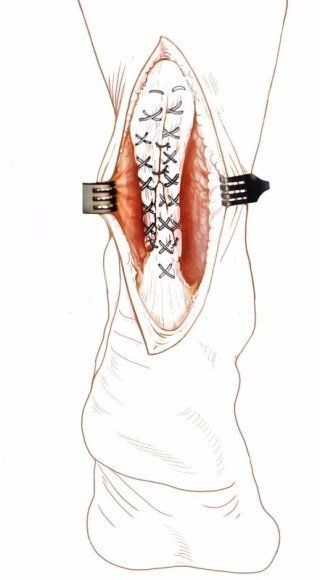
Complete tendon rupture
In the case of complete tendon rupture, depending on the type of injury, surgical treatment involves direct repair of the Achilles tendon in acute ruptures. If the injury is not recent and the residual damaged tissue is insufficient for direct tendon repair, reinforcement repair is performed, using the turnover of the calf fascia or an adjacent tendon (Short Peroneal or Long Flexor of the big toe), which is inserted to strengthen the repaired portion.
Postoperative treatment is crucial for functional recovery.
Recent studies show that early rehabilitation, with well-defined protocols and good collaboration between the surgeon, physiatrist, and physiotherapist, leads to better results, especially in patients with high functional demands.