Pseudoarthrosis
Pseudoarthrosis
Pseudoarthrosis is the failure of a fracture to heal.
Every fracture that occurs in our body has the potential to heal correctly but also the risk of non-consolidation. The bone consolidation phase is a biological process influenced by many factors, some biological and others mechanical. The main biological factor is blood supply, while the mechanical factor is stability.
All bone segments can undergo pseudoarthrosis, although the most frequently involved are the femur, tibia, humerus, ulna, radius, scaphoid, astragalus, and the fifth metatarsal bone.
Classification
For the choice of treatment, it is useful to divide pseudoarthrosis into non-infected and infected.
Non-infected pseudoarthrosis
Non-infected pseudoarthrosis can be divided into mobile or fixed. This distinction can be made after a simple physical examination that assesses the stability of pseudoarthrosis; if the movement during manipulation is extensive, the pseudoarthrosis will be mobile, if the movement is minimal, the pseudoarthrosis will be fixed.
Pseudoarthrosis can be radiographically classified as atrophic or hypertrophic. The former is associated with poor vascular supply, and the latter with a lack of mechanical stability. In atrophic pseudoarthrosis, there are few signs of bone apposition, sometimes there may be resorption of the ends, and usually, the bone segment is mobile.
In hypertrophic pseudoarthrosis, there is an increase in bone callus at the fracture site, with signs of consolidation without complete healing, and usually, there is less mobility.
Infected pseudoarthrosis
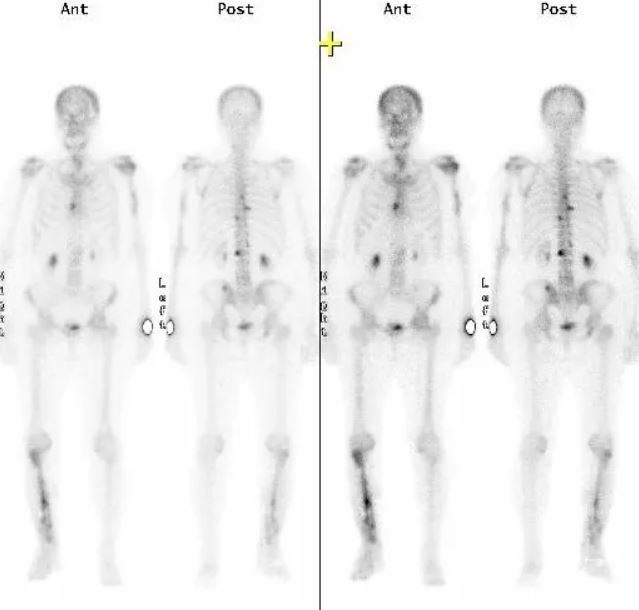
If pseudoarthrosis is infected, the bacteria present within the fracture site pose an additional obstacle to bone healing. Infection can lead to an increase in local temperature, swelling, and redness of the skin. Bone infection can be confirmed by an elevation in inflammatory markers, a scintigraphy with marked leukocytes, or a positron emission tomography.
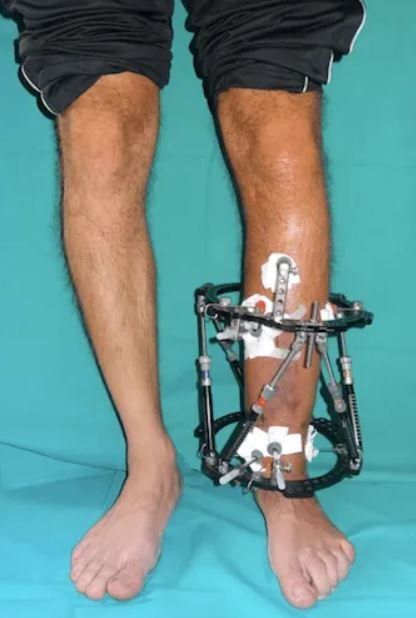
Treatment usually requires meticulous surgical cleaning of the fracture site and removal of necrotic bone, which causes shortening of the bone segment. This shortening can be recovered using distraction osteogenesis, a technique involving the application of an external fixator to gradually lengthen the affected bone segment until complete recovery of length.
Bone healing
After a fracture is treated, new bone tissue begins to form to reconnect the bone fragments. For proper bone healing, stability, blood supply, and adequate nutrition are necessary.
Stability
All non-surgical or surgical treatments for bone repair follow a basic rule: the fractured bone segment must be realigned, and the movement of the two fragments must be limited until complete healing. Some fractures, especially if complex, can be held in place with casts or splints; others require more stable surgical fixation, which can be achieved with intramedullary nails, plates, screws, or external fixators.
Blood supply
Blood carries essential components for healing to the fracture site, including oxygen, nutrients, bone repair cells, and growth factors. Blood supply to the bone injury usually returns on its own during the healing period.
Nutrition
Having a healthy and balanced diet plays a crucial role in bone healing. This involves consuming foods high in protein, calcium, vitamin C, and D. Dietary supplements beyond daily requirements are not necessary (a rare exception is for severely malnourished patients with metabolic disorders or multiorgan damage. In this case, the doctor will advise on the best dietary guidelines and potentially add nutritional supplements).
Causes
Pseudoarthrosis occurs when the bone lacks sufficient stability, blood flow is reduced, or in the presence of severe metabolic deficiencies. Pseudoarthrosis is more frequent as a result of high-energy traumas, such as a car accident, as these severe injuries often compromise vascularization, and some are exposed, meaning the bone segment comes into contact with contaminants external to the skin, increasing the risk of infection.
Other causes may include:
Interposition of soft tissues between the two bone fragments
Significant bone loss
Damage to the surrounding muscles and soft tissues
Mechanical distraction at the fracture site.
Causes related to treatment:
Insufficient reduction
Stability of synthesis
Inadequate immobilisation
Errors in the application of synthesis means.
Risk factors
Some factors that increase the risk of pseudoarthrosis.
Advanced age
Alcohol
Smoking
Tissue hypoperfusion
Severe anaemia
Diabetes
Hyperparathyroidism
Hypothyroidism
Low levels of vitamin D
Poor nutrition
Use of corticosteroids, acetylsalicylic acid, ibuprofen
Infection
A fracture with complications
Blood supply
Pseudoarthrosis is more likely if the damaged bone has limited blood supply.
Some bones, like those in the foot, have intrinsic stability and excellent blood supply. In these cases, fractures may heal with non-surgical treatment.
Other bones, like the femoral head, talus, and scaphoid, have limited blood supply. In these cases, a fracture can cause a disruption in the vascular system, increasing the risk of pseudoarthrosis.
Finally, other bones, like the tibia, have moderate blood supply as they are covered by a thin layer of soft tissues. Severe trauma can compromise both internal and external vascularisation, increasing the risk of pseudoarthrosis.
Symptoms
Patients with pseudoarthrosis usually experience pain at the fracture site long after the traumatic event.
This pain may persist for months or years and can be constant or only occur when the affected bone is used.
Clinical examination
To diagnose pseudoarthrosis, the orthopaedic specialist must perform a thorough physical examination and assess the stability of the fracture-affected segment.
Instrumental exams
The most useful exams for the diagnosis and follow-up of pseudoarthrosis are:
X-rays
Computed Tomography (CT)
Magnetic Resonance Imaging (MRI)
Pseudoarthrosis is diagnosed when clinical and radiographic examinations show no progression of bone healing after 6 months from the fracture.
Blood tests can be used to identify deficiencies in vitamins, calcium, anaemia, diabetes, or ongoing infection.
Non-surgical treatment
The most common non-surgical treatment is performed using a plaster cast or an external brace, in the case of a closed pseudoarthrosis. The use of PEMF (pulsed electromagnetic fields) or shock wave stimulation can be helpful.
Surgical treatment
Surgery is mandatory for infected pseudoarthrosis and necessary for non-infected cases when non-surgical methods fail or in the mobilisation of previously implanted synthesis means. A second surgical intervention might be necessary if the first one fails to heal the fracture. The main surgical options include:
- Distraction of the pseudoarthrosis focus
- Compression of the pseudoarthrosis focus
- Revision of the pseudoarthrosis focus with removal of necrotic bone tissue
Frequently, the use of bone grafts is necessary for:
- Filling bone gaps
- Reactivating the healing process (Autologous bone grafts)
- Structural support (Homologous Bone Graft - Opposed bone splints)
Autologous Bone Graft
In this procedure, the bone is taken from the patient, usually from a donor site such as the pelvis, and transplanted to the fracture site. This allows fresh bone cells and growth factors to initiate the healing process of pseudoarthrosis. Although the removal of the bone may be painful, the quantity removed does not lead to functional, structural, or aesthetic problems.
Homologous Bone Graft
In a homologous graft, the bone comes from a bone bank. After harvesting from the donor, the bone is processed for implantation and control. Choosing these grafts allows the patient to avoid pain at the donor site and has the advantage of having larger bone segments available. However, this choice involves a longer integration time and a higher risk of infection.
Surgical treatment options include:
- Internal fixation: Orthopaedic surgeons use intramedullary nails, metal plates, and screws to stabilise pseudoarthrosis. Often, bone grafts are used to assist stability and promote healing.
- External fixation: Orthopaedic surgeons apply an external device to the affected limb using steel wires and pins. This method is preferred for pseudoarthrosis without sufficient stability, infected cases, or those with bone loss.
Recent technical innovations have led to the development of more advanced external fixators that allow axial correction of deformities and bone healing, utilising osteogenic distraction. These fixators, called Hexapods, have transformed external fixation, making it simpler and easier for patients to manage. By gradually changing the length of 6-millimetre rods, the patient can autonomously correct axial deviations and lengthen the bone segment if necessary.